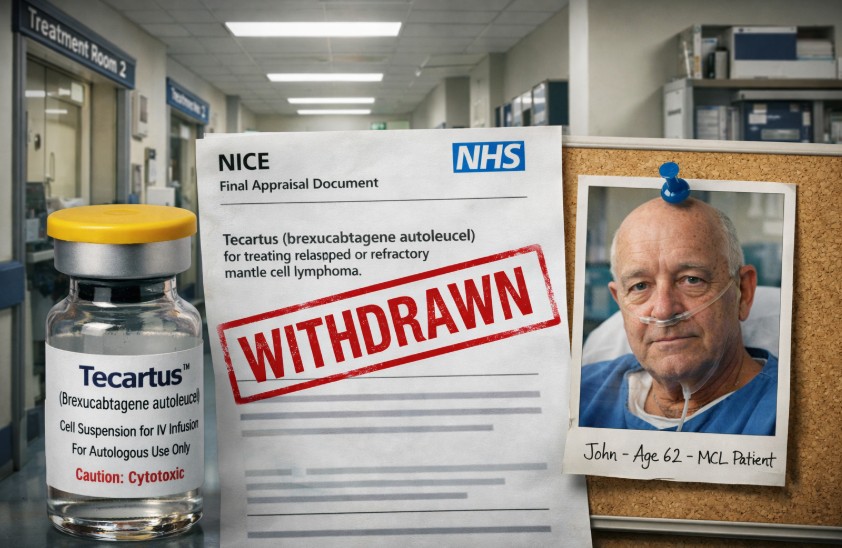
The NHS watchdog’s decision to withdraw Tecartus, a life-saving CAR T-cell therapy, has sparked widespread concern across the UK. Experts, charities, and patients alike are calling it a step backward in cancer care, especially for those with few or no other options.
Tecartus was a vital treatment for relapsed mantle cell lymphoma patients, offering renewed hope where standard therapies failed. Its removal from NHS funding has ignited public outcry and triggered a formal appeal.
Key Takeaways:
- NICE ruled Tecartus ineffective in real-world use compared to trial results
- The treatment was the only CAR T-cell option for mantle cell lymphoma
- Blood cancer charities and patients have appealed the decision
- Alternatives are under review but not yet approved
- The move raises ethical and clinical concerns about NHS cancer care
What Is Tecartus and Why Was It Offered Through the NHS?

Tecartus was introduced as a cutting-edge therapy within the NHS to treat a specific group of cancer patients facing limited options. As the only CAR T-cell treatment available for relapsed or refractory mantle cell lymphoma in the UK, it represented a major advancement in blood cancer care. The NHS facilitated access to this high-cost therapy through a special funding route, offering new hope to patients with aggressive disease profiles.
Overview of Tecartus (brexu-cel)
Tecartus, commercially known as brexucabtagene autoleucel or brexu-cel, is a personalised immunotherapy treatment developed by Kite, a Gilead Company. It was designed to treat mantle cell lymphoma (MCL), a rare and fast-progressing form of non-Hodgkin lymphoma that predominantly affects older adults.
This therapy works by collecting the patient’s T-cells (a type of white blood cell) and genetically modifying them to express a receptor that can identify and destroy cancerous B-cells. After the cells are engineered, they are re-infused into the patient’s bloodstream to begin attacking cancer cells directly.
Key points about Tecartus:
- It is a CAR T-cell therapy, a form of advanced immunotherapy.
- Approved for patients aged 26 and above with relapsed or refractory MCL.
- Offers a personalised and targeted approach, unlike chemotherapy.
- Intended for patients who have not responded to at least two prior therapies.
Tecartus marked a significant step in tailored cancer treatments, especially for rare blood cancers with limited therapeutic options.
CAR T-cell Therapy and Its Use in Mantle Cell Lymphoma
Chimeric Antigen Receptor T-cell (CAR T-cell) therapy is a revolutionary form of treatment in oncology. It uses the body’s immune system to fight cancer by modifying a patient’s own T-cells to better recognise and kill cancerous cells.
In the case of mantle cell lymphoma:
- CAR T-cell therapy has shown potential for inducing deep remission, even in patients with advanced-stage disease.
- It is particularly valuable for relapsed or refractory cases, where standard treatments like chemotherapy or stem cell transplants have failed.
- Tecartus was the only CAR T-cell therapy licensed for MCL in the UK at the time of its NHS rollout.
This treatment gave patients a final option when other methods had been exhausted, providing a chance at long-term remission.
Cancer Drugs Fund and Conditional NHS Availability
Due to its high cost and limited early data, Tecartus was made accessible through the Cancer Drugs Fund (CDF), a special NHS funding mechanism that supports access to promising cancer drugs while additional evidence is gathered.
How the CDF worked in this case:
- Tecartus was conditionally approved in England and Wales.
- The fund allowed patients to receive the drug while NICE monitored real-world outcomes.
- Data collected from these patients informed future decisions on routine NHS use.
This approach helped bridge the gap between innovation and affordability, making Tecartus available for those in urgent need while maintaining clinical oversight.
Tecartus’s introduction into the NHS highlighted both the promise of modern cancer therapy and the complexity of balancing innovation with policy and cost.
What Prompted the NHS Watchdog to Withdraw Tecartus?
The National Institute for Health and Care Excellence (NICE), the body responsible for evaluating the cost-effectiveness of treatments in the UK, determined that Tecartus underperformed in NHS clinical settings. This conclusion was based on nearly five years of real-world data collected through the Cancer Drugs Fund.
NICE found that Tecartus did not deliver the same outcomes in practice as seen in clinical trials. Specifically, the median survival rate for patients using Tecartus in trials was four years, while NHS data showed a lower median survival of 2.5 years.
Based on this, NICE deemed the treatment less clinically beneficial than previously thought and concluded that it did not provide sufficient value for its cost to justify continued NHS use.
Although recognising the treatment’s potential, NICE ultimately recommended against its ongoing availability within the NHS, sparking widespread backlash and calls for reconsideration.
Who Is Most Affected by the Tecartus NHS Watchdog Decision?
The decision primarily impacts adults in the UK diagnosed with relapsed or refractory mantle cell lymphoma, a rare and aggressive blood cancer. The condition affects around 600 people annually, with many depending on Tecartus as their last remaining treatment option after multiple therapies have failed.
Patients aged 26 and older who were eligible for this therapy now face an uncertain future, particularly those who are no longer responding to chemotherapy or stem cell transplants. For many, Tecartus was a lifeline when all standard treatments had failed, offering a genuine chance at remission and a better quality of life.
Patients like Paul Madley, a 66-year-old from Cardiff, are examples of individuals who benefited significantly from the therapy. Madley achieved remission after Tecartus treatment and returned to an active lifestyle, making the sudden withdrawal of access to such care devastating for similar patients.
The withdrawal also affects NHS oncologists and haematology specialists who must now find alternative options, often with lower success rates.
Why Are Cancer Charities and Experts Challenging the Decision?
The NICE ruling triggered immediate objections from leading blood cancer charities and healthcare professionals who argue that it disregards real patient impact and limits vital treatment options.
Key voices in opposition include:
- Blood Cancer UK: Submitted a formal appeal questioning NICE’s evaluation process
- Lymphoma Action: Highlighted growing concern and anxiety among patients
- Anthony Nolan: Called the decision “deeply disappointing” and damaging to patient outcomes
Many experts believe that real-world NHS data does not fully reflect the therapy’s potential, as variables in implementation may have affected results. They also raise concerns that the economic model used by NICE underestimates the long-term benefit for those who do respond positively.
Health professionals on the frontlines have also noted firsthand improvements in patient lives, including prolonged remission and recovery stories. These advocates argue that the evaluation process must better consider individual patient responses and the absence of effective alternatives for this specific cancer type.
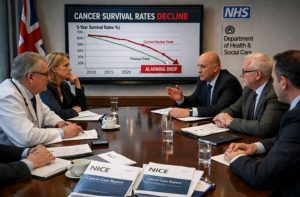
Is Removing Tecartus a “Backward Step” in UK Cancer Care?

The removal of Tecartus from the NHS has been widely viewed as a concerning reversal in the fight against aggressive blood cancers. Experts argue that it reflects deeper issues in how the healthcare system evaluates life-saving innovations, especially when dealing with rare conditions like mantle cell lymphoma.
The Uniqueness of Tecartus as the Only CAR T-cell Option
Tecartus was the only CAR T-cell therapy approved for mantle cell lymphoma in the UK. This uniqueness made it a crucial part of the treatment pathway for patients with no other viable options. Its targeted mechanism provided hope for long-term remission, even in cases resistant to chemotherapy or stem cell transplants.
Concerns About NHS Regression in Life-saving Treatments
Many see the decision as a regression in NHS cancer care standards. Dr Rubina Ahmed from Blood Cancer UK expressed concern about what the decision means for patients with limited alternatives, pointing out that such high-impact treatments should remain accessible while evidence continues to develop. Removing a potentially curative option based solely on cost-effectiveness and incomplete data undermines patient care advancements.
- Access to Tecartus symbolised NHS support for innovative treatments
- The withdrawal may deter future adoption of cutting-edge therapies
- Patients currently in remission fear their progress may be disregarded in policy shifts
Public Sentiment and Media Framing
The public reaction has been one of frustration, disbelief, and sadness. Stories like Paul Madley’s, who attributes his remission to Tecartus, demonstrate the real, lived benefits of the therapy.
His account of recovery and return to a normal life contrasts starkly with the clinical language of “insufficient effectiveness.” Media outlets and social platforms have amplified such patient stories, framing the NICE decision as bureaucratic overreach disconnected from on-the-ground reality.
Overall, the decision challenges the public’s trust in NHS prioritisation and raises broader ethical questions about valuing patient lives in cost-based systems.
What Alternatives to Tecartus Are Being Considered by NICE?
Following the decision to discontinue Tecartus, NICE is currently evaluating two alternative treatments for mantle cell lymphoma: sonrotoclax and acalabrutinib.
These therapies are in the process of review but have not yet been approved for NHS use in this context. NICE has noted that both could present promising options in the future, but their long-term effectiveness and cost-efficiency must be thoroughly assessed.
In the meantime, patients are left with fewer treatment paths, typically involving additional rounds of chemotherapy, which may have lower success rates. Until alternative therapies are approved and made available, the treatment gap left by Tecartus remains a significant challenge for clinicians and patients alike.
What Happens Next? Appeal Process and Potential Reinstatement

The decision by NICE to remove Tecartus is currently under formal appeal, lodged by major cancer charities and advocacy organisations. This appeal seeks to challenge the methods used in NICE’s evaluation and to request a re-examination of the evidence, particularly focusing on patient impact and specialist feedback.
NICE has acknowledged the appeal and stated that it will follow its established review process to consider the points raised. The outcome of this appeal could lead to reinstatement, modification of the access criteria, or further clarification about the future of CAR T-cell therapy within the NHS.
In the meantime, patients already undergoing treatment with Tecartus will be allowed to complete their course. The appeal offers a potential pathway to restoring access, but the timeline and outcome remain uncertain.
What Does This Mean for the Future of NHS Cancer Treatment?
The Tecartus decision underscores growing tension in NHS policy between medical innovation and cost-driven regulation. It raises important questions about how treatments for rare diseases are evaluated and who ultimately decides what defines value in healthcare.
Key considerations include:
- Balancing cost-efficiency with clinical need in rare cancers
- Supporting patient-first approaches in treatment evaluation
- Encouraging continued investment in personalised therapies
NICE’s role as a gatekeeper means its decisions carry immense weight, and cases like Tecartus may lead to pressure for reform in how real-world data and patient outcomes are factored into assessments. Future policies may need to shift towards greater flexibility, particularly in evaluating complex treatments with promising but varied results.
This decision may serve as a turning point, sparking necessary discussions around NHS priorities, funding structures, and access to groundbreaking care. How it is handled will shape public trust in the system moving forward.
Conclusion
The removal of Tecartus from NHS availability has ignited widespread concern, from patients and medical professionals to national charities.
As the only CAR T-cell therapy approved for mantle cell lymphoma, its withdrawal creates a substantial gap in treatment options for a small but vulnerable patient population.
While NICE based its decision on real-world data showing reduced effectiveness, the move has been criticised for overlooking patient success stories and the urgent need for effective alternatives.
A formal appeal is now underway, offering a glimmer of hope that access may be reconsidered. Until then, the situation remains deeply unsettling for those who saw Tecartus as a final chance at life.
This decision is more than just a clinical judgment, it’s a defining moment for the NHS and its approach to innovative cancer care in the UK.
FAQs
What is Tecartus used to treat?
Tecartus is a CAR T-cell therapy used to treat relapsed or refractory mantle cell lymphoma, a rare and aggressive type of blood cancer.
Why did NICE withdraw Tecartus from the NHS?
NICE concluded that Tecartus did not perform as well in NHS settings as it did in clinical trials and was not cost-effective based on updated survival data.
Who can currently receive Tecartus treatment on the NHS?
Only patients who had already begun Tecartus treatment prior to the decision can complete their therapy under the NHS.
Is there an appeal against the Tecartus withdrawal?
Yes, charities like Blood Cancer UK and Anthony Nolan have filed a formal appeal challenging NICE’s evaluation and requesting a review.
Are there any alternatives to Tecartus currently available?
While NICE is reviewing other treatments such as sonrotoclax and acalabrutinib, no equivalent CAR T-cell therapy is available right now.
How many people are affected by this decision in the UK?
Approximately 600 people are diagnosed with mantle cell lymphoma each year in the UK, many of whom may have relied on Tecartus.
What is the main concern from cancer experts about this decision?
Experts argue that removing Tecartus limits access to the only advanced therapy for certain patients and could set a worrying precedent for future innovations.